Who Benefits? Equity Questions about Cognitive Enhancers
A student in a late-night library wonders if a pill levels the playing field or deepens divides; narrative frames who gains and who loses.
Low-income students, workers juggling multiple jobs, and those without medical access may be excluded, raising clear equity and justice concerns.
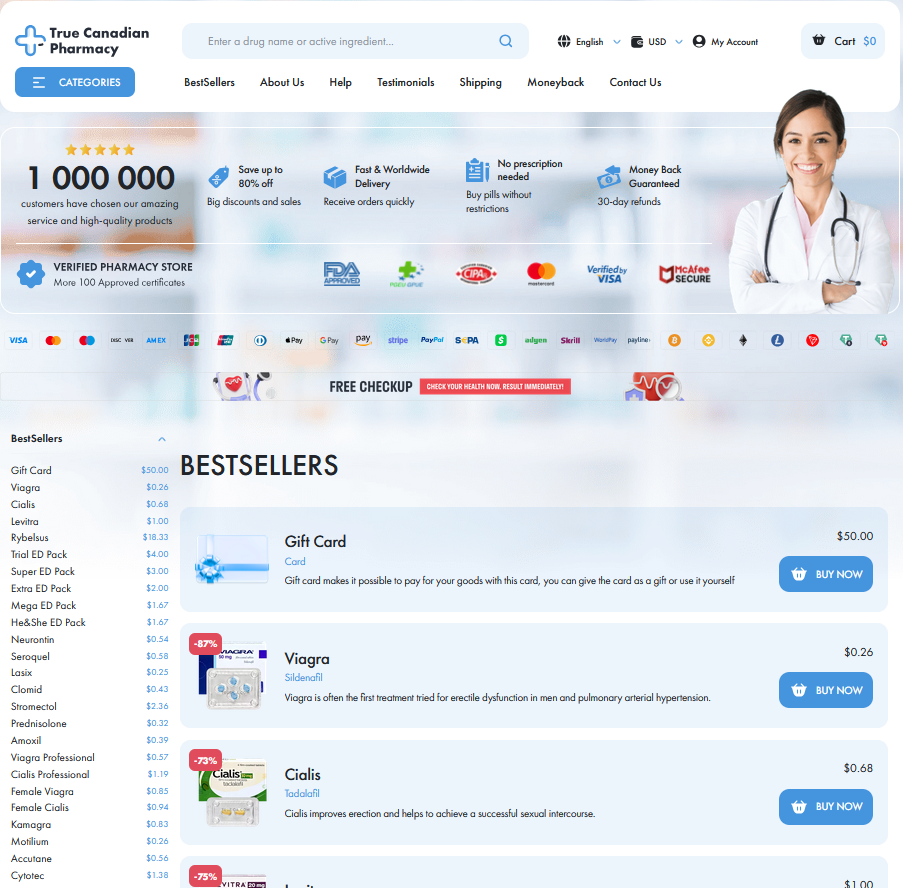
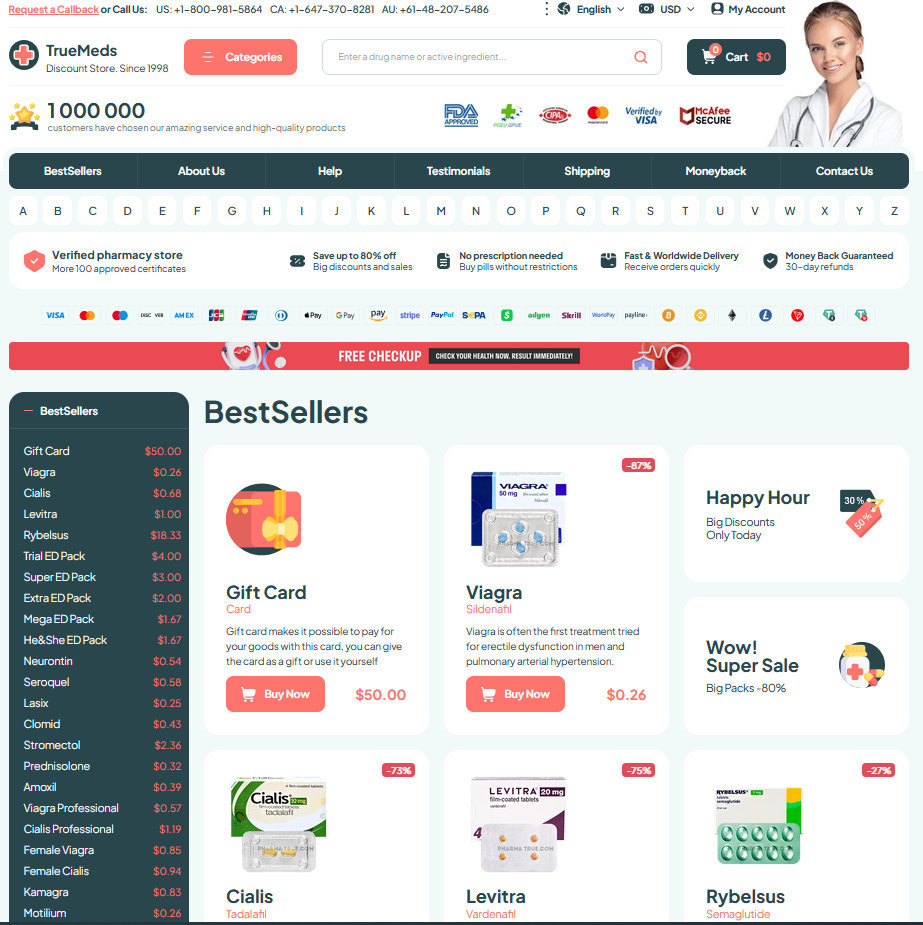
Insurance gaps, prescription hurdles, and cultural stigma make enhancement uneven; some aquire advantages while others risk punishment for informal use.
Policy must balance safety, accessibility, and fairness; education, regulated provision, and workplace safeguards could help, but debate remains definately unresolved for many communities and professions today.
Cheating or Coping? Reframing Academic Stimulant Use

On a late-night campus walk, a classmate confesses to using provigil to get through endless readings — not to game grades but to keep up with a crushing workload. Framing this behavior as merely cheating flattens a complex human story: students juggle jobs, family obligations, and uneven access to resources. We should ask who can aquire prescriptions, who resorts to black-market pills, and how institutions can respond without shaming coping strategies.
Ethical debate moves from blame to policy when we consider disparities and harms: provigil may offer short-term focus but carries unknown long-term effects and can normalize an always-on enviroment. Universities might combine education about risks, accessible mental health care, and clear amnesty policies for disclosure. Such steps respect autonomy, reduce inequity, and maintain academic integrity by treating stimulant use as a public-health issue rather than a simple honor-code violation.
Hidden Harms: Long-term Health Versus Quick Wins
A grad student recalls the first all-nighter when a peer offered provigil for focus. That quick win felt like a miracle, yet slowly seeded a habit of reliance.
Clinical trials show short-term attention gains, but long-term neurochemical effects remain poorly understood. Risks to sleep architecture, impulse control, and mood over years of repeated use definately worry clinicians.
Users report bursts of productivity, yet provigil can mask burnout and unmet supports; occasional dependency might develop, and some adverse effects occassionally surface only after months of routine use.
A balanced approach asks for monitoring, longer follow-up studies, and transparent patient education. Institutions should prefer harm-reduction strategies, accommodate underlying needs, and resist normalizing enhancement without data or adoption.
Employer Oversight: Privacy, Disclosure, and Reasonable Accommodation

Teh corridor conversations about provigil blur legality and empathy: an employee confides they use it to meet deadlines, and HR must weigh confidentiality against safety. Privacy laws limit invasive screening, so employers should focus on function and risk assessment rather than probing motives.
Clear policies can balance disclosure and accommodation, offering medical channels for those who need support and precise performance standards that dont penalize reasonable choices. Employers should avoid surveillance-heavy responses, prefer narrow, evidence-based guidelines, and Acommodate legitimate needs while ensuring fairness and workplace safety and protect worker dignity.
Societal Pressures, Workplace Culture, and Normalized Enhancement
In open-plan offices and late-night libraries a quiet current runs beneath routines: people reach for provigil to sustain focus. The scene feels heroic but often masks subtle coercion.
Norms shift as small choices compound; what begins as voluntary aid becomes an unstated baseline. Workers compare output, hours, and attention as metrics that reward constant availability and edge-seeking.
Addressing this requires cultural shifts: clearer expectations, realistic deadlines, and supportive policies so individuals can choose without pressure. Occassionally small gestures — flexible hours or workload reshaping — matter, and mental wellbeing too, and balance.
| Item | Note |
|---|---|
| provigil use | Normalization risk |
Policy Proposals: Navigating Regulation, Consent, and Fairness
Policymakers must balance access and oversight, designing clear rules that reduce coercion without criminalizing self-care. Equity and accountability should guide any licensing or distribution choices for students and workers alike.
Consent regimes should be robust: informed, revocable, and sensitive to power imbalances. Goverment policies ought to distinguish therapeutic use from performance pressure, with clear reporting safeguards and independent oversight bodies.
Regulation should embed research mandates and equitable access funds, enabling long-term safety monitoring and subsidies for under-resourced communities to avoid market-driven escalation and protect public institutional trust. PMC review MedlinePlus