How Periactin Works to Increase Appetite
In everyday clinical stories, patients describe a gentle return of appetite after starting cyproheptadine. Teh drug acts as an antihistamine and a serotonin antagonist, blocking 5-HT2 and H1 receptors and dampening central satiety pathways. This biochemical shift often restores hunger signals that had been suppressed by illness, stress, or medications.
Clinically, blocking 5-HT2 receptors reduces serotonin’s anorectic signal in hypothalamic circuits, while H1 antagonism loosens histamine-linked satiety. Together these central effects, plus peripheral changes in gastric motility and nausea reduction, create a permissive state for increased intake. Patients often note more frequent hunger cues.
These actions come with sedative and anticholinergic side effects that may increase appetite indirectly by reducing nausea and improving sleep, but they can be problematic in some settings. Monitor for drowsiness, dry mouth, and rare cardiac changes, especially in frail patients or in a constrained enviroment.
| Receptor | Primary effect |
|---|---|
| 5-HT2 | Blocks anorexigenic serotonin |
| H1 | Reduces histamine-related satiety |
Evidence Summary: Clinical Studies and Real-world Experience

Clinical trials and observational series paint a nuanced picture: periactin often stimulates appetite and weight gain in short-term studies of cachexia, pediatric failure-to-thrive, and chemotherapy-associated anorexia. Response rates vary, with measurable increases in caloric intake within days; benefits are usually modest but meaningful for frail patients. Placebo-controlled trials provide most of the objective data.
In practice, clinicians report rapid appetite improvement but caution about sedation, dry mouth, and weight distribution changes; adverse effects are usually mild and Occassionally limit use. Dosage varies by age and condition, and off-label use is common. Combining periactin with dietary plans and close follow-up maximizes benefit, while periodic reassessment helps balance gains against side-effect burden and aligns expectations for families.
Dosage Options, Timing, and Practical Administration Tips
I once counseled a patient who struggled to eat; we discussed starting low and moving slow to find balance. Small, consistent doses often yield clearer results without overwhelming side effects.
Clinicians typically begin with conservative amounts and adjust based on response and tolerability. For many, bedtime dosing helps reduce daytime drowsiness while supporting overnight appetite gains.
When using periactin, track intake, weight, and symptoms in a simple log. Make adjustments slowly and involve caregivers so changes are noticed and documented; this helps to Recieve useful feedback.
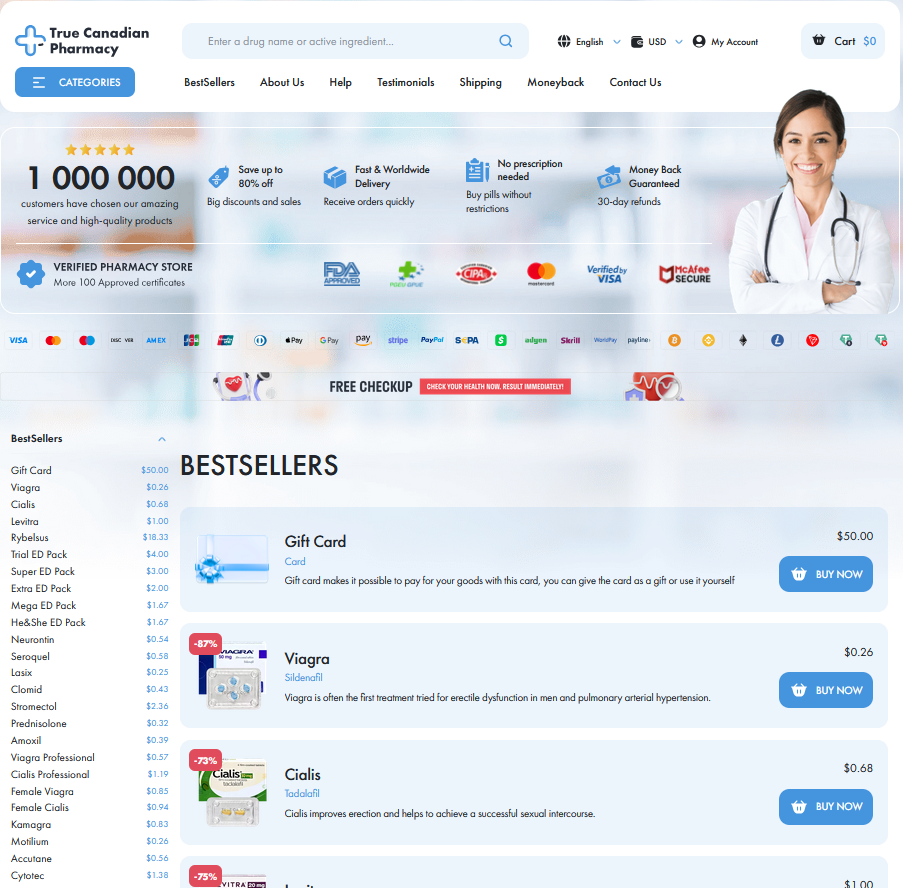
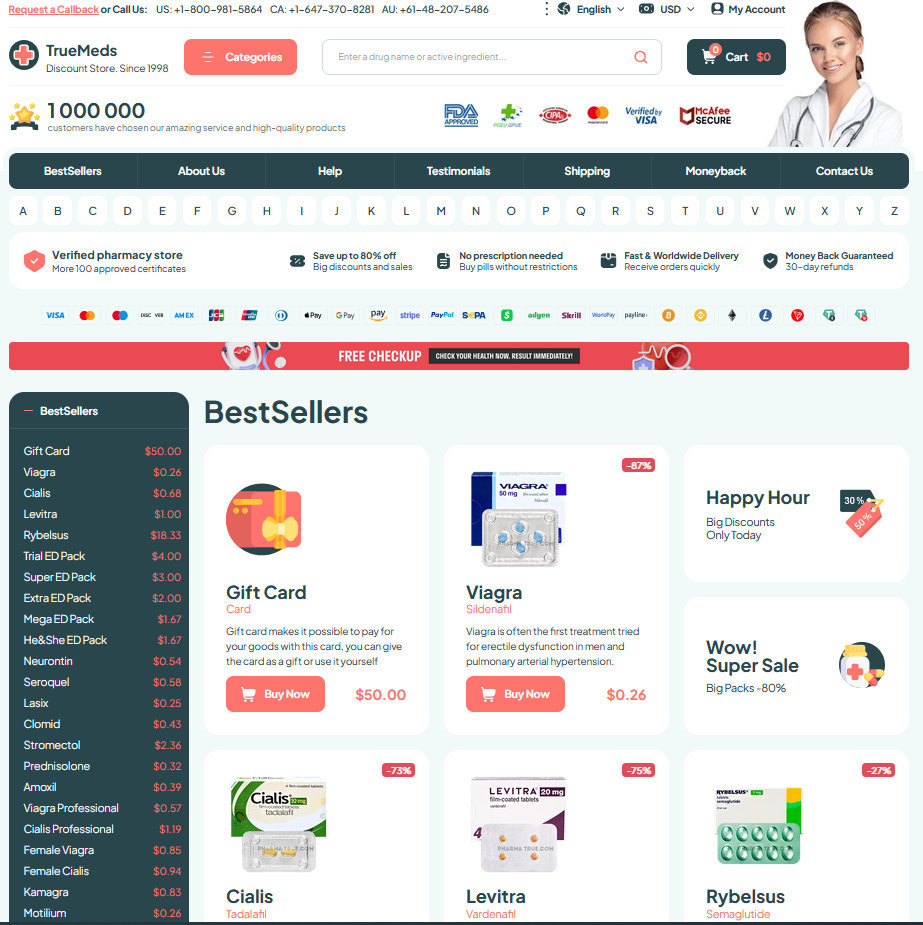
Practical tips include taking doses with food if nausea appears, avoiding alcohol, and learning how to aquire affordable supplies. Discuss any concerns with a prescriber before altering your plan.
Managing Side Effects and Safety Precautions Effectively

When starting periactin, expect mild drowsiness, dry mouth, or weight gain — simple signals that call for gentle monitoring. Keep a log of appetite, sleep, and mood, and share it with your clinician; medication reviews help spot interactions early.
If side effects persist, dose reduction or alternate-day schedules can be tried under supervision. Avoid alcohol and sedatives, and watch for rare allergic reactions or changes in mood that need urgent review. Occassionally labs or ECGs are suggested for those with cardiac risk; always ask questions until you fully Aquire confidence.
Who Benefits Most: Patient Profiles and Considerations
A caregiver's note often opens the discussion: a modest periactin prescription returned appetite and ease to daily life when medical causes were treated. Ideal candidates include older adults with unexplained weight loss, children with failure to thrive, and patients recovering from surgery or chronic illness where short term stimulation can restore strength.
Clinicians monitor benefits and sedative effects, tailoring duration and dose, and consider interactions and contraindications. Use is Occassionally avoided in those with liver disease or uncontrolled asthma. Shared decision making, nutritional support, and short trials with clear goals help Acomplish overall safe, patient-centered therapy.
| Profile | Why |
|---|---|
| Cachexia | Stimulates appetite |
Combining Periactin with Nutrition and Lifestyle Strategies
Think of the medication as one tool within a feeding plan: increased hunger needs structure to become gains. Pair doses with favorite nutrient-dense foods, set regular small meals, and use sauces or spices to rekindle pleasure and intake over time.
Time dosing to when appetite returns most — morning or evening — and keep a simple food log for two weeks. Choose energy-dense options like nut butters, full-fat dairy, smoothies, and fortified snacks to convert extra eating into calories and protein.
Add light resistance exercise, maintain good sleep, and build pleasant mealtime cues. Watch for sedation or digestive changes; discuss them with your clinician if noticable. Adjust intake gradually and personalize plan over months. MedlinePlus StatPearls